What are the Parkinson’s Plus Syndromes?
It is best to think of the Parkinson’s Plus syndromes as the sisters of Parkinson’s disease.
Although many diseases are similar to Parkinson’s disease, the changes they produce and their symptoms are slightly different. It’s why we think of these diseases as the sisters of Parkinson’s disease.
Another name for them is the “Parkinson’s Plus” syndromes.
![Parkinson's Plus Syndromes [5 important mimics] 2 Sisters](https://cdn5440.templcdn.com/wp-content/uploads/2019/04/Sisters-500x333.jpg)
There are three common Parkinson’s Plus syndromes.
2. Multiple System Atrophy (MSA)
3. Cortico Basal Degeneration (CBD)
Ideally, the specific Parkinson’s Plus Syndrome should be identified correctly before the start of treatment.
But in the early stages of the disease, this may be difficult, and sometimes impossible. You ca read more here [external link: Frontiers in Neurology].
Because it is sometimes impossible to tell PSP, MSA, and CBD apart, doctors sometimes diagnose the patient as having a “Parkinson’s Plus” syndrome without noting the specific disease.
As the years go by, the appearance of characteristic features (such as eye movement problems in PSP) may enable your doctor to make a more precise diagnosis.
Which Symptoms May Indicate a Parkinson’s Plus Syndrome?
If you have any of the following features, you may have a Parkinson’s Plus syndrome. These features are called “red flags”. This means that if you have one of these symptoms, your doctor is supposed to pause and think.
![Parkinson's Plus Syndromes [5 important mimics] 3 Red flags tell your doctor that you may have one of the Parkinson's Plus syndromes.](https://cdn5440.templcdn.com/wp-content/uploads/2019/04/red-flag-3132583_1920-e1575817892956-500x331.jpg)
2. Frequently falling down, especially backwards.
3. Severe talking or swallowing problems.
4. Problems with eye movement.
5. Impotence.
6. Blurring of vision.
7. Blacking out when rising from a seated position.
8. Problems with thinking or memory loss.
9. Personality changes.
10. Symptoms only in the legs while the arms and hands are completely normal.
11. Rapid progression of the disease
What is the Treatment for a Parkinson’s Plus Syndrome?
The treatment for a Parkinson’s Plus syndrome is the same as the treatment for Parkinson’s disease itself.
Many patients respond to Levodopa. However, what’s challenging is that sometimes Levodopa does not have a dramatic effect. It may also happen that this effect may not last for many years. Therefore, the response to levodopa is somewhat unpredictable.
![Parkinson's Plus Syndromes [5 important mimics] 4 LevodopaToDopamine](https://cdn5440.templcdn.com/wp-content/uploads/2019/04/LevodopaToDopamine-500x115.png)
That being said, a significant proportion of patients with Parkinson’s Plus syndromes respond positively to a comprehensive treatment effort. This effort should include the treatment of special problems associated with each syndrome. Therefore, it is crucial to figure out which kind of Parkinson’s Plus syndrome early you have so that these specific problems can be treated.
For example:
- In PSP, the patient frequently falls backwards because the areas of the brain responsible for balance are not functioning well. In this case, balance training can help.
- In MSA, the patient can fall because of a drop in blood pressure when they get up. In this case, they should drink enough water and try to get up slowly to prevent falls. Some medications can also prevent falls.
What is Progressive Supranuclear Palsy (PSP)?
PSP is the most common of the “Parkinson’s Plus” syndromes. Patients with PSP frequently fall backwards.
To know more about PSP, click here: [PSP patient guide]
What is Multiple System Atrophy (MSA)?
MSA is the second most common of the “Parkinson’s Plus” syndromes. Patients with MSA have trouble with a part of their nervous system that controls blood pressure, heart rate, sweating and sexual function.
To know more about MSA, click here: [MSA in detail]
What are Other Types of Parkinson’s Plus Syndromes?
There are many other Parkinson’s Plus Syndromes. Since it’s not possible to describe each of these in detail here, I will mention their names and certain key characteristics.
- Corticobasal Degeneration: Characterized by difficulty using automatic movements of an arm or hand.
- Dementia with Lewy Bodies: Characterized by hallucinations & disorganized behaviour.
- Frontotemporal dementia (“Pick’s disease”): Characterized by personality changes, including impulsivity and dis-inhibition.
Here is a nice review of many Parkinson’s Plus Syndromes. It is very nicely written, but a bit detailed: [McFarland et al 2016, Neurology Continuum].
| Caution: This information is not a substitute for professional care. Do not change your medications/treatment without your doctor's permission. |
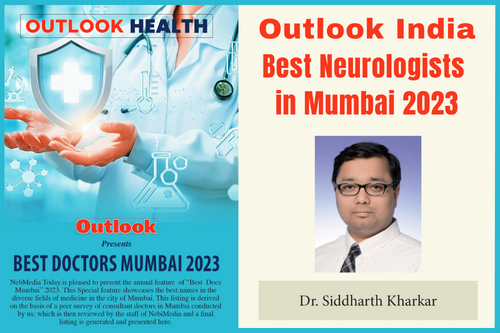
 Dr. Siddharth KharkarDr. Siddharth Kharkar has been recognized as one of the best neurologists in Mumbai by Outlook India magazine and India today Magazine. He is a board certified (American Board of Psychiatry & Neurology certified) Neurologist. Dr. Siddharth Kharkar is a Epilepsy specialist in Mumbai & Parkinson's specialist in Mumbai, Maharashtra, India. He has trained in the best institutions in India, US and UK including KEM hospital in Mumbai, Johns Hopkins University in Baltimore, University of California at San Francisco (UCSF), USA & Kings College in London. |
 Skip to content
Skip to content
![Parkinson's Plus Syndromes [5 important mimics] 1 red flag 3132583 1920 e1575817892956](https://cdn5440.templcdn.com/wp-content/uploads/2019/04/red-flag-3132583_1920-e1575817892956.jpg)